Abstract
This paper provides a comprehensive overview of ultrasound stimulation, focusing on its physics, interactions with the human body, and biological effects. The physics of ultrasound, including parameters such as wavelength, frequency, velocity, and amplitude, are explained. The diverse biological effects of ultrasound on cellular responses, tissue regeneration, and neural activity modulation are explored. The thermal and non-thermal mechanisms through which ultrasound produces biological effects, such as heating, radiation force, and cavitation, are explained.
Introduction
Ultrasound stimulation is the use of sound waves at a frequency higher than the upper limit of human hearing (typically above 20 kHz) for therapeutic or diagnostic purposes [1]. It is a mechanical wave in the form of molecular vibrations, which transfer energy from one position to another [2]. In medicine, ultrasonic waves have a frequency of 1-20 MHz. Ultrasound has a mired type of application in medicine. The most common clinical application of that is for safe, non-invasive medical imaging. In addition, it has many other uses in medicine, such as stimulation [3]. You can visit our papers [4] [5] [6] for more information about various stimulation.
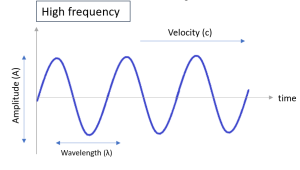
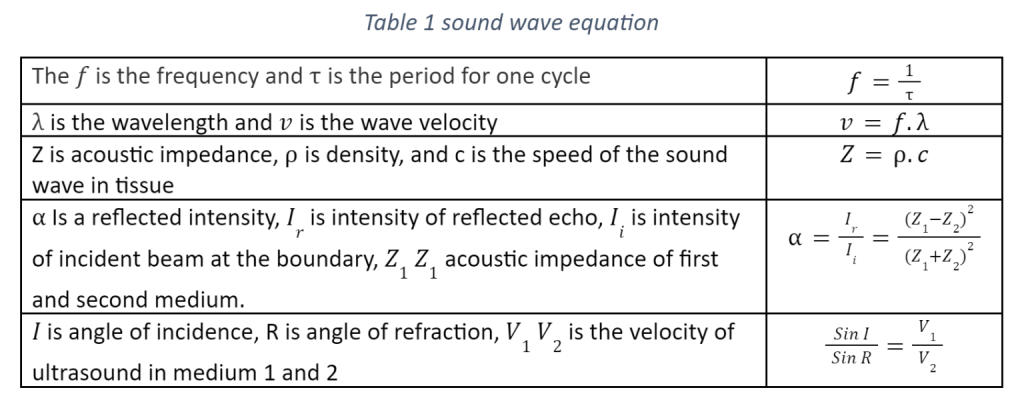
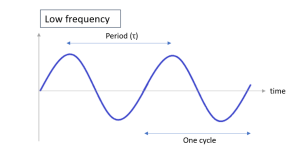
This paragraph provides a brief explanation of the physics of ultrasound and its behavior in the human body. Understanding the physics of ultrasound requires an appreciation of several key parameters, including wavelength, frequency, velocity, and amplitude. The amplitude represents the maximum disturbance a wave can cause, while the frequency is the number of oscillations per second, and the wavelength on the other hand, is the distance between two points of the same phase. The time it takes for one complete cycle is known as the wave’s period, and velocity is the rate at which a wave travels through a medium in meters per second. Table 1 provides the equations for these parameters.
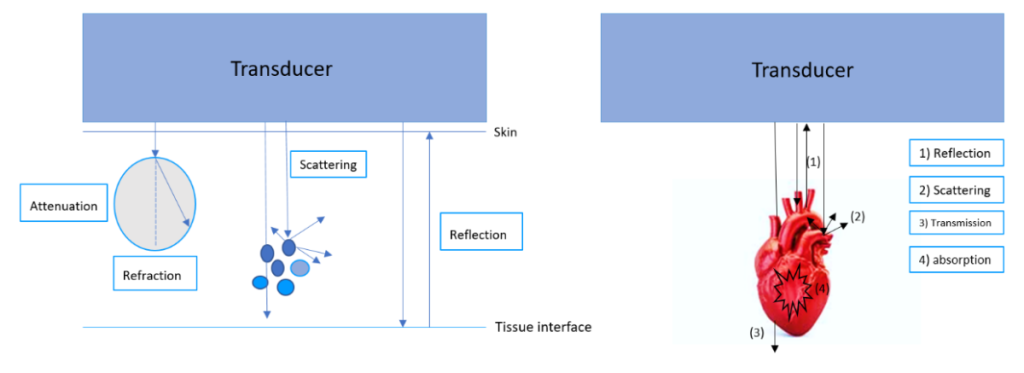
Figure 1, also illustrates the differences between high and low frequency waves. High-frequency waves have short periods, while low frequency waves penetrate deeply into the body, reaching many organs. To apply ultrasound as a stimulation or other application, the beam must be emitted into the tissue. Once it travels through the tissue, ultrasound is characterized by various features. The interaction processes are affected by the features of the ultrasonic wave and the physical characteristics of the tissues that the beam passes through [7].
Reflection
When an ultrasonic wave travels through one material and finds another with a different acoustic impedance and propagation qualities, such as fat, muscle, and blood, it will not transmit it, and reflection occurs under the law of reflection that regulates sound. The acoustic impedance differential between the two media determines how much reflection occurs. The reflected ultrasound waves can be targeted on a particular target, such a tumor, to destroy it or stimulate surrounding tissue. This reflection effect is also used in therapeutic ultrasound. This is comparable to how light waves reflect when they come into contact with a mirror. The equation of reflected intensity is shown in table 1. [8]
Refraction
When ultrasound travels through two different mediums with varying velocities, refraction occurs at the boundary where the beam direction changes. As the ultrasound passes through the first medium and into the second, its wavelength changes, yet its beam frequency doesn’t. Refraction follows Snell’s law, and its equation can be seen in Table 1.
Attenuation
Attenuation is a loss of energy from sound waves. Basically, attenuation is the damping of sound, an interruption that diminishes the volume and quality of the sound wave. The interaction of sound waves with tissue and tissue boundaries results in attenuation for a number of reasons. Watts/cm2 is a unit of measurement for the space-averaged intensity of ultrasound produced by a transducer. This attenuation is caused by absorption, scattering, and reflection of the ultrasound energy as it interacts with the medium. The mechanical energy of the sound wave is transformed into heat and absorbed by the tissues, which is the leading cause of ultrasonic wave attenuation. The second most frequent cause of attenuation is the scattering of ultrasonic waves, with reflection, interference, divergence, and diffraction having just a little contribution. These two elements lower the ultrasonic beam’s intensity to the point where it is decreased to half at a particular depth below the surface. The attenuation observed when a tissue sample is interposed between a source and receiver may be affected by reflection, refraction, and phase distortion in the wave transmitted through the sample as shown in the Figure 2. [9]
Scattering
The incident ultrasound beam is reflected in a broad range of directions when the reflecting interface has an irregular shape and has smaller dimensions than the ultrasonic beam’s diameter. Non-specular reflection or scattering is the technical term for this. It is known as scattering. Scattering occurs when an ultrasonic sound wave encounters a structure with a smaller wavelength and a different acoustic impedance from the surrounding tissue. The minor surface imperfections of visceral organs and red blood cells are two examples of “diffuse reflectors,” or elements that induce scatter. Scattering can be seen in Figure 2. [10]
Absorption
Absorption of ultrasound is the process of conversion of vibrational energy into heat as it passes through a medium such as tissue [11]. The absorption of the ultrasound in soft tissues occurs at the macromolecular level [9]. The frequency of the wave, the characteristics of the medium, and the wave’s course through the medium all affect how much ultrasonic energy is absorbed. While lower frequency ultrasonic waves penetrate tissue more deeply but are less effectively absorbed, higher frequency ultrasound waves are absorbed more quickly and have a lesser penetration depth. Both diagnostic and therapeutic uses of ultrasound absorption exist, including the removal of tumors and the disintegration of kidney stones. Diagnostic uses of ultrasound absorption include the evaluation of tissue features.
Ultrasound in Medicine: Biological Effects, Models, and Applications
Ultrasound has been utilized in medicine for many years because of its non-invasive and safe effects. Over time, ultrasound technologies have undergone significant changes in how they are used in tissue, cell, and nerve regeneration, as well as in modulating neural activity. This section explores the diverse biological effects of ultrasound and its applications in various medical fields.
Bio-effect of Ultrasound
Ultrasound stimulation has been shown to have various biological effects on cells and tissues, including increased cellular metabolism, improved cell proliferation and differentiation, including apoptosis and modulating intracellular signaling pathways, and enhanced tissue regeneration. It has also been demonstrated to modulate neural activity, promote blood flow, and reduce inflammation, although it is not really obvious how sound waves interact with neural tissue at the cellular or molecular level. In this paragraph, we discuss several of the potential explanations that have been put up to account for the function of US.
Mechanisms of Ultrasound’s Biological Impact
Ultrasound’s ability to produce biological effects in tissue is attributed to both thermal and non-thermal mechanisms [12] . The non-thermal mechanisms can be divided into radiation force and acoustic cavitation. Therefore, heating, radiation force, and acoustic cavitation are three ways that the US can have biological impact [13].
Thermal Effect of Ultrasound
The thermal effect of ultrasound can be either harmful or beneficial. Due to absorption and scattering, energy is lost in an attenuating pattern as ultrasound traverses tissue, and this energy is turned into heat. When the amount of energy produced is greater than the amount of scattered heat, the temperature of the tissue increases, resulting in the thermal effect of ultrasound.
The thermal effect will have a cell death in the area with minimal damage to the surrounding tissues. The volume of the lesion can vary depending on the type of equipment and ultrasound used. Multiple lesions can be merged to cover the complete volume of bigger entities such as tumors [14] [15]. Figure 3 depicts the region of cell death. This effect can modulate brain function through irreversibly denaturing proteins or reversibly lowering synaptic transmission. The extent of this heat-induced neuronal modulation depends on several factors, including tissue density, ultrasound frequency, intensity, duration, and speed of sound. By adjusting these parameters, it is possible to either suppress or activate neuronal activities [16]. Besides the bioactivity of organelles and chemical transfer at synaptic connections are both influenced by temperature. So, the excitability of the neurons can be increased; however, in the high intensities, synaptic transmission, tissue homogenization, protein denaturation, and DNA fragmentation will be decreased [16].
![Figure 3) Thermal Effect of ultrasound on tissue. When the US passes through the tissue the amplitude diminishes due to the converting energy into the heat [14] [20]](https://allostasis.io/wp-content/uploads/2023/06/Screenshot-177-300x136-1.png)
Cavitation
Acoustic cavitation is a process of creating microbubbles in liquid or liquid-like material using high frequency ultrasound. When ultrasound waves travel through tissue with a strong tensile phase, submicron-sized vapor and/or gas pockets initially dissolved in the medium can be pulled out to create tiny bubbles [17]. These cavities oscillate, expand and finally collapse when subjected to sufficiently large sound pressures. This process is called non-inertial cavitation, and it has been shown to influence the potential of a cell’s membrane and the bilayer lipid membrane, causing it to deform and create intramembrane microbubbles [18]. In contrast, inertial cavitation occurs when the liquid’s inertia causes bubble motion and collapse, generating high pressures and temperatures that can be destructive to tissue. This type of cavitation is utilized in therapeutic applications, such as tissue ablation, cell lysis, and drug delivery, but it can also cause unwanted tissue damage and should be carefully controlled and monitored. The threshold for inertial cavitation depends on factors such as acoustic pressure, temperature, and frequency and can vary depending on the tissue type and location.

Acoustic Radiative Forces (ARFs)
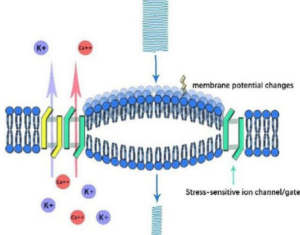
Acoustic radiation force (ARF) is a phenomenon in which ultrasound waves exert a force that pushes objects in the direction of the beam. ARFs find applications in various fields, including biomedical research and material science. One effect of ARFs is the stretching of cell membranes, which can impact the conformational states of molecules connected to the membrane, such as ion channels [19]. The static pressure generated by ARFs can alter the capacitance of the cell membrane, affecting nerve activity by mechanically activating stress-sensitive ion gates and channels, and modifying membranous potential and capacitance [16] [18]. ARFs have also been found to play a crucial role in the production of endothelial nitric oxide, which controls ion channel activity. Furthermore, specific types of ultrasound can activate voltage-gated sodium and calcium channels, leading to action potentials and synaptic transmission [20] [21]
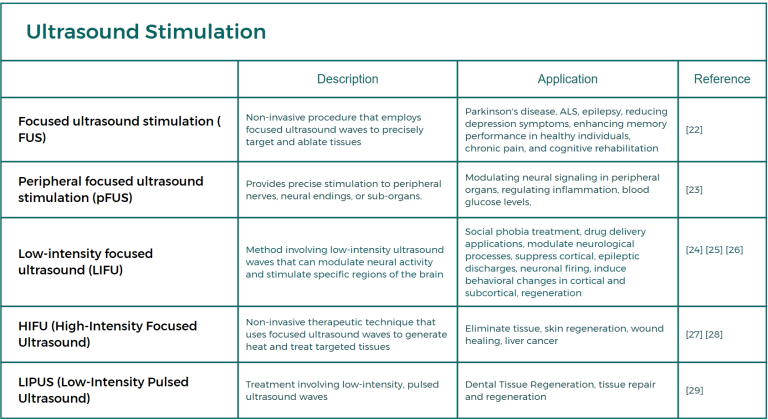
Different Types of Ultrasound Stimulation and Their Applications
Ultrasound stimulations encompass various types, each serving distinct purposes. These include Focused Ultrasound Stimulation (FUS), Peripheral Focused Ultrasound Stimulation (pFUS), Low-Intensity Focused Ultrasound (LIFU), Low-Intensity Pulsed Ultrasound (LIPUS), and High-Intensity Focused Ultrasound (HIFU). Table 1 presents concise definitions and examples of applications for these stimulation methods. For a comprehensive understanding with detailed information, readers are encouraged to refer to paper 2, which provides an in-depth exploration of these ultrasound stimulation techniques.
Table 2 Types of ultrasound stimulation
Conclusion
Ultrasound Stimulation has emerged as a valuable and safe tool with numerous applications, thanks to its non-invasive nature. This paper provides a comprehensive understanding of the physics of ultrasound and its behavior within the human body, shedding light on the interaction between ultrasound waves and tissues. The study explores the diverse biological effects of ultrasound, including cellular responses, tissue regeneration, and modulation of neural activity. It delves into the thermal and non-thermal mechanisms underlying these effects, such as heating, radiation force, and cavitation. Gaining a thorough understanding of the biological impact of ultrasound is essential for its successful application across various fields. Future papers will delve into different types of ultrasound stimulation and their specific uses, providing in-depth insights into this rapidly advancing field.
References
- https://doi.org/10.1155/2013/269724
- http://dx.doi.org/10.15412/J.BCN.03070303
- https://doi.org/10.3389/fncel.2021.812588
- https://www.allostasis.io/photobiomodulation-therapy-in-peripheral-nerve-system/
- https://www.allostasis.io/transcranial-electrical-stimulation/
- https://www.allostasis.io/electrical-stimulation/
- https://doi.org/10.1016/j.mpaic.2018.01.005
- https://doi.org/10.1016/j.mpaic.2020.11.012
- https://doi.org/10.1121/1.386254
- http://info.isradiology.org/docs_books/basic/Chapter3.pdf
- https://doi.org/10.1016/0301-5629(75)90124-6
- https://doi.org/10.3390/genes11091086
- https://doi.org/10.1007/s13534-016-0007-y
- https://d3nqfeqdtaoni.cloudfront.net/images/pdf/Bioeffects_Paper_July_2015.pdf
- https://doi.org/10.1111/j.1442-2042.2011.02936.x
- http://dx.doi.org/10.15412/J.BCN.03070303
- https://doi.org/10.1523%2FENEURO.0136-15.2016
- https://doi.org/10.1103/PhysRevX.4.011004
- https://thejns.org/doi/abs/10.3171/2017.11.FOCUS17621
- https://doi.org/10.3389/fphys.2020.00787
- https://doi.org/10.15412/j.bcn.03070303
- https://doi.org/10.1016/j.brs.2022.01.014
- https://doi.org/10.1038/s41467-019-08750-9
- https://doi.org/10.1093/cercor/bhac037
- https://doi.org/10.3389/fpsyt.2022.825802
- https://www.researchgate.net/publication/51510371_A_review_of_low-intensity_focused_ultrasound
- https://doi.org/10.1038/s41598-021-81878-1
- https://doi.org/10.1002/cncr.25192
- http://dx.doi.org/10.1016/j.joen.2015.12.019