HRV Signal Acquisition
Required hardware characteristics
Electrodes
Firstly, ECG data were collected using Ambu white sensor 4500M-H. Then conductive textile and thread were used to acquire data.
Sensor and Processor modules

The hardware consists of two main modules: Sensor board and Processor board. In sensor part 8 pieces of analog single-lead ECG front end, AD8232, is used, which supports 1 to 8-channel of ECG measurement. As seen in hardware configuration, fig.1, the analog to digital converter, the microcontroller processor and the bluetooth module are compartments of a board constructed based on Nano 33 BLE sense.
Recording Protocol
Depending on application, different recording protocols with various number of electrodes can be opted. 2-electrode system for ECG registration records one lead by using 2 electrodes and is particularly useful for heart rate and heart rate variability tracking. 3-electrode system uses three electrodes (RA, LA and LL) and the monitor displays the bipolar leads (I, II and III). Also, as figure 4 illustrates, the augmented leads can be estimated [1]. For boosting the signal and noise reduction, a reference electrode should be added to the system [1]. In 5-electrode system, the monitor displays 6 leads (I, II, III, aVF, aVL and aVR) by using 5 electrodes (RA, RL, LA, LL and chest).
Sensor Placement
Depending on the type of wearables different sensor placements to find the best place of ECG acquisition have been proposed by different research works.
In 2020, li et al. represented the optimal 3-electrode placement for wearable devices, which have most direction-based similarity as cardiac vector. In the below picture, this system is depicted. In this system, electrode 1 is negative, electrode 2 is positive and third one refers to the reference electrode [3].
In wearable devices motion artifact is the most detrimental noise added to the ECG. Based on research in presence of nine different types of motions, including arm motions in sagittal, frontal and horizontal plane directions and three bodice movements: forward flexion, backward flexion and rotation of the spine, the most stable electrode positions are as shown in fig. 3. ECG recording wearables can be designed in accordance with this result [4].

In addition to thoracic recordings, one to three leads ECG can be recorded from arm. Various armbands are being utilized for clinical/research purposes, despite the fact that it is more affected by movements.
In [6], a new wearable device for ECG monitoring was developed. The device was placed on the left upper arm and worn as an armband. Besides this device can simultaneously record three ECG channels and one EMG channel.
Generally, the placement of electrodes in armbands is shown in fig 6 The ground electrode should be placed on interior part and positive and negative sensors on exterior (upper) part of the left arm.

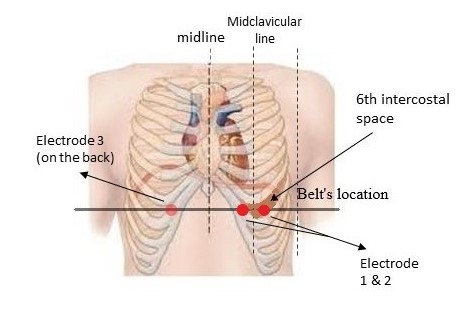
The other possible wearable to record ECG signal is a belt. An electrode belt was used to record the ECG in [5]. The electrode belt was placed on the 6th intercostal space’s horizontal line, with electrodes 1 and 2 placed on the left and right mid-clavicular lines, and electrode 3 was utilized to decrease common mode noise and was placed on the person’s back. Based on the effective and low complexity motion artifact removal method (see part (b)), this sensor placement, fig 5, could be one of the best choices.
References
[1] P. Kligfield et al., “Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology,” Journal of the American College of Cardiology, vol. 49, no. 10, pp. 1109-1127, 2007.
[2] B. J. Drew et al., “Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and cardiovascular disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses,” Circulation, vol. 110, no. 17, pp. 2721-2746, 2004.
[3] M. Li, W. Xiong, and Y. Li, “Wearable measurement of ECG signals based on smart clothing,” International journal of telemedicine and applications, vol. 2020, 2020.
[4] H. Cho and J. H. Lee, “A study on the optimal positions of ECG electrodes in a garment for the design of ECG-monitoring clothing for male,” Journal of medical systems, vol. 39, no. 9, pp. 1-14, 2015.
[5] X. An and G. K Stylios, “Comparison of motion artefact reduction methods and the implementation of adaptive motion artefact reduction in wearable electrocardiogram monitoring,” Sensors, vol. 20, no. 5, p. 1468, 2020.
[6] J. T. Bigger, J. L. Fleiss, L. M. Rolnitzky, and R. C. Steinman, “The ability of several short-term measures of RR variability to predict mortality after myocardial infarction,” (in eng), Circulation, vol. 88, no. 3, pp. 927-34, Sep 1993.